Press Releases
September 9, 2019
Juntendo University Corporate Communications
Juntendo University Research
IPS based approach for treating virus-induced tumors
(Tokyo,9 September) In a recent study published in the journal Haematologica, researchers at Juntendo University used stem cell technology to produce immune cells with an enhanced ability to fight aggressive tumors of the nasal cavity
A lesser known but invasive form of cancer prevalent in Asian countries is extranodal natural killer/T cell lymphoma (ENKL). While it starts within the nasal cavity it often spreads to the digestive system, kidneys and bone marrow. At present, the enzyme L-asparaginase is the only therapy available for treating ENKL. However, many patients do not respond well to L-asparaginase thereby greatly decreasing their chances of prolonged survival. Now, researchers at Juntendo University have created “customized” cells that show promise in reducing the size of tumors in model mouse experiments.
T-cells are an important component of the immune system and protect the body against disease. They can detect special proteins of the surface of pathogens, thereby recognizing and remembering all invaders. Since ENKL tumors are commonly infected with the Epstein-Barr virus (EBV), T-cells recognize these tumor cells by the presence of viral proteins. However, T-cells continuously exposed to EBV-infected ENKL tumors eventually age and lose their ability to fight. To create younger and stronger T-cells, the research team used stem cell technology.
Stem cells can be modified to create any kind of specialized cells of the body. T-cells from patients’ blood, which were accustomed to identifying ENKL tumors, were first collected and then genetically modified into stem cells. These stem cells were then used to create a batch of newly-produced T-cells subsequently named as rejuvenated T-cells (rejTs). RejTs were not only younger but already had ENKL-tumor recognition ingrained into them. Their ability to attack tumors was investigated next.
The researchers found that not only did the rejTs correctly recognize and reduce the size of the tumor cells but did so more efficiently than the original T-cells. Similar results were observed when rejTs were injected into mice with ENKL tumors. The team also noted that all organs examined in mice were tumor free after only three injections of rejTs. Unlike the original T-cells the rejTs acted fast and relentlessly. Lastly, rejTs were tested in combination with anti–PD-L1 antibodies that are used in a highly effective new class of anti-cancer drugs. However, rejTs given to the mice with and without anti–PD-1 antibodies had very similar effects. The anti-cancer effects of rejTs were so strong that using anti–PD-1 antibodies was redundant.
This study showed a promising new treatment option for ENKL patients. "Our results collectively suggest that to treat relapsed and refractory ENKL using LMP1- and LMP2-specific rejTs will be very useful," concludes the research team. The fact that rejTs can be synthesized from stem cells in unlimited numbers is an added bonus.
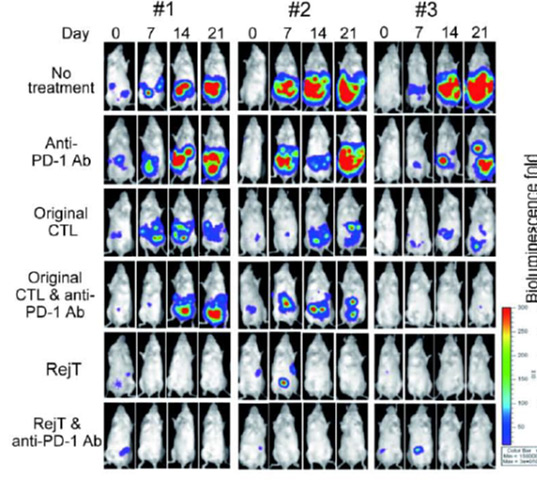
Figure 1. RejT cells resulted in an almost complete disappearance of ENKL tumors in mice, compared to the original T-cells and anti–PD-L1 antibodies.
Background
Stem cells
Stem cells are typically found in the bone marrow and blood of adult humans and can be transformed to create any required cell in the body. On the other hand, induced stem cells, which were used in this study, can be reverse-engineered from regular body cells by reprogramming their genes. Induced stem cells thus can give rise to an infinite number of the required cells, while retaining some properties of the parent cells used to create them.
Reference
Miki Ando, Jun Ando, Satoshi Yamazaki, Midori Ishii, Yumi Sakiyama, Sakiko Harada, Tadahiro Honda, Tomoyuki Yamaguchi, Masanori Nojima, Koichi Ohshima, Hiromitsu Nakauchi, and Norio Komatsu. Long-term eradication of extranodal NK/T cell lymphoma, nasal type, by induced pluripotent stem cell-derived Epstein-Barr virus-specific rejuvenated T cells in vivo. Haematologica, July 2019.
DOI: 10.3324/haematol.2019.223511
http://www.haematologica.org/content/early/2019/07/09/haematol.2019.223511

