The animal responsible for causing the most human deaths each year is neither lions, sharks, nor snakes. By far, the world's deadliest animal is the mosquito (Gatesnote). The majority of these deaths are caused by malaria, a major disease transmitted by mosquitoes. At the Department of Tropical Medicine and Parasitology, Juntendo University School of Medicine, we are conducting research on malaria.
1. Malaria and the Problems It Causes_
- ・What is Malaria?_
- ・Efforts Toward Malaria Elimination and the Challenges to Overcome_
- ・Drug Resistance—When Treatments No Longer Work_
2. Our Ongoing Research: "Offensive" Malaria Drug Resistance Research_
- Field Research_
___1) What we have discovered so far – Discovery of Artemisinin-resistant Parasites in Africa______
___2) Moving forward – Expanding on Our Field Discoveries
______
- Laboratory Research_
__ 1) Validating Field Findings and Developing New Techniques for Early Detection of Resistant Parasites
2) Predicting the Future – Developing a System to Predict Future Drug-resistant Parasites in the Field
______
3. Conclusion_
1. Malaria and the Problems It Causes
・What is Malaria?![]() Malaria is one of the world's three major infectious diseases, alongside HIV/AIDS and tuberculosis. It is caused by a parasite called the malaria parasite, transmitted through the bite of an infected mosquito. Of the types of malaria parasites that infect humans, the ones most likely to cause death are widely distributed in Africa and around the world. Malaria once existed in Japan, but after the implementation of malaria eradication programs focusing on controlling mosquito vectors, as well as infrastructure improvements such as roads and waterways, malaria epidemics ended in the 1950s. However, malaria continues to cause significant issues in many countries. In Africa, malaria is as common as the cold or flu in Japan. Worldwide, there are hundreds of millions of new malaria cases annually, with 420,000 deaths. Malaria hinders economic development, which in turn exacerbates the spread of the disease. Malaria and development are inextricably linked. Eradicating malaria breaks this vicious cycle and contributes significantly to sustainable development.
Malaria is one of the world's three major infectious diseases, alongside HIV/AIDS and tuberculosis. It is caused by a parasite called the malaria parasite, transmitted through the bite of an infected mosquito. Of the types of malaria parasites that infect humans, the ones most likely to cause death are widely distributed in Africa and around the world. Malaria once existed in Japan, but after the implementation of malaria eradication programs focusing on controlling mosquito vectors, as well as infrastructure improvements such as roads and waterways, malaria epidemics ended in the 1950s. However, malaria continues to cause significant issues in many countries. In Africa, malaria is as common as the cold or flu in Japan. Worldwide, there are hundreds of millions of new malaria cases annually, with 420,000 deaths. Malaria hinders economic development, which in turn exacerbates the spread of the disease. Malaria and development are inextricably linked. Eradicating malaria breaks this vicious cycle and contributes significantly to sustainable development.
____
・Efforts Toward Malaria Elimination and the Challenges to Overcome![]() Various global efforts are underway to eliminate malaria. Malaria spreads through the bite of infected mosquitoes. To control this, effective methods include distributing insecticide-treated nets (ITNs) and spraying long-lasting insecticides indoors (IRS). Additionally, malaria can be prevented through early treatment, and the effectiveness of current treatments has led to a decline in malaria-related deaths since the mid-2000s.
Various global efforts are underway to eliminate malaria. Malaria spreads through the bite of infected mosquitoes. To control this, effective methods include distributing insecticide-treated nets (ITNs) and spraying long-lasting insecticides indoors (IRS). Additionally, malaria can be prevented through early treatment, and the effectiveness of current treatments has led to a decline in malaria-related deaths since the mid-2000s.![]() However, there are limitations in combating the mosquito vectors, which dominate the ecosystem on a much larger scale than the malaria parasite. The malaria parasite, which has been in an evolutionary battle with humans for hundreds of thousands of years, is highly intelligent and uses various strategies to ensure its survival. If an effective vaccine is developed, it could shift the paradigm of malaria elimination strategies. However, the malaria parasite has evolved numerous mechanisms to escape human immunity, making the development of a vaccine extremely difficult. To date, no sufficiently effective vaccine has been developed. Furthermore, a more serious situation is emerging in the form of drug resistance—malaria parasites that are no longer affected by current treatments. We are advancing basic and innovative applied research to address this issue. Details are provided below.
However, there are limitations in combating the mosquito vectors, which dominate the ecosystem on a much larger scale than the malaria parasite. The malaria parasite, which has been in an evolutionary battle with humans for hundreds of thousands of years, is highly intelligent and uses various strategies to ensure its survival. If an effective vaccine is developed, it could shift the paradigm of malaria elimination strategies. However, the malaria parasite has evolved numerous mechanisms to escape human immunity, making the development of a vaccine extremely difficult. To date, no sufficiently effective vaccine has been developed. Furthermore, a more serious situation is emerging in the form of drug resistance—malaria parasites that are no longer affected by current treatments. We are advancing basic and innovative applied research to address this issue. Details are provided below.
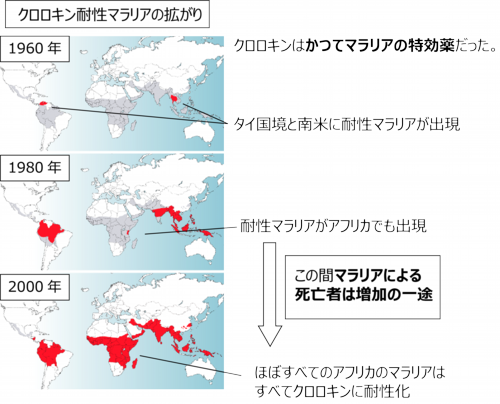
・Drug Resistance—When Treatments No Longer Work![]() The emergence of drug-resistant pathogens is one of the most troublesome issues in the battle against diseases. In addition to malaria, drug-resistant microorganisms are a significant global problem, and it is predicted that by 2050, drug-resistant infections will cause more deaths than cancer. The same issue applies to malaria. Even when new drugs are developed, drug-resistant parasites eventually emerge. For example, chloroquine, once a highly effective malaria treatment, saw resistance emerge by the late 1950s, and by the 1980s, the resistant parasites had spread throughout Africa.
The emergence of drug-resistant pathogens is one of the most troublesome issues in the battle against diseases. In addition to malaria, drug-resistant microorganisms are a significant global problem, and it is predicted that by 2050, drug-resistant infections will cause more deaths than cancer. The same issue applies to malaria. Even when new drugs are developed, drug-resistant parasites eventually emerge. For example, chloroquine, once a highly effective malaria treatment, saw resistance emerge by the late 1950s, and by the 1980s, the resistant parasites had spread throughout Africa.
____
2. Our Ongoing Research: "Offensive" Malaria Drug Resistance Research
![]() To solve the problem of drug resistance, it is essential to discover new insights through
research and develop new technologies. Since our lab restructured in 2012, we have
focused on malaria drug resistance as the cornerstone of our research and have made
significant achievements. Our goal is to use basic research to clarify the mechanisms of
resistance and the evolutionary mechanisms of resistance, and based on these insights, to
develop effective countermeasures against drug resistance. Our research is based on two
main pillars: field research, which involves surveys in the affected regions, and laboratory-
based molecular biological research. Here, I will briefly explain what we are doing in both
areas.
To solve the problem of drug resistance, it is essential to discover new insights through
research and develop new technologies. Since our lab restructured in 2012, we have
focused on malaria drug resistance as the cornerstone of our research and have made
significant achievements. Our goal is to use basic research to clarify the mechanisms of
resistance and the evolutionary mechanisms of resistance, and based on these insights, to
develop effective countermeasures against drug resistance. Our research is based on two
main pillars: field research, which involves surveys in the affected regions, and laboratory-
based molecular biological research. Here, I will briefly explain what we are doing in both
areas.
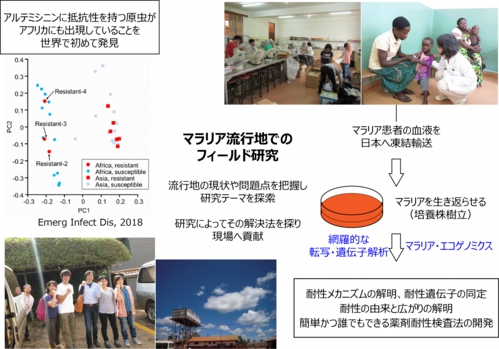
・Field Research![]() Field research allows us to explore solutions to drug resistance from a
macro perspective. Our lab regularly conducts drug resistance surveys in Uganda and
Papua New Guinea. Together with other universities and research institutes, we form teams
that stay on-site for 1-2 months, conducting ongoing surveys to evaluate the effectiveness
of malaria drugs in these regions. These surveys have been ongoing since 2013 in Uganda
and since 2016 in Papua New Guinea. Both are tropical countries located along the
equator, with a large number of malaria patients.
Field research allows us to explore solutions to drug resistance from a
macro perspective. Our lab regularly conducts drug resistance surveys in Uganda and
Papua New Guinea. Together with other universities and research institutes, we form teams
that stay on-site for 1-2 months, conducting ongoing surveys to evaluate the effectiveness
of malaria drugs in these regions. These surveys have been ongoing since 2013 in Uganda
and since 2016 in Papua New Guinea. Both are tropical countries located along the
equator, with a large number of malaria patients.
1) What we have discovered so far – Discovery of Artemisinin-resistant Parasites in Africa![]() Our field surveys have led to several new discoveries. One such discovery,
achieved through our ongoing surveys in Uganda, is the identification of Artemisinin-
resistant parasites. Artemisinin, an anti-malarial drug, quickly eliminates the malaria
parasite and alleviates symptoms. It is currently used as the first-line drug in all malaria-
endemic countries, and its introduction has led to a decline in malaria-related deaths since
the mid-2000s. The Nobel Prize in Physiology or Medicine was awarded to Tu Youyou in
2015 for her remarkable contribution to tropical medicine.
Our field surveys have led to several new discoveries. One such discovery,
achieved through our ongoing surveys in Uganda, is the identification of Artemisinin-
resistant parasites. Artemisinin, an anti-malarial drug, quickly eliminates the malaria
parasite and alleviates symptoms. It is currently used as the first-line drug in all malaria-
endemic countries, and its introduction has led to a decline in malaria-related deaths since
the mid-2000s. The Nobel Prize in Physiology or Medicine was awarded to Tu Youyou in
2015 for her remarkable contribution to tropical medicine.
However, in countries along the Mekong River, such as Cambodia and Myanmar,
Artemisinin-resistant parasites have already emerged. Special testing methods are required
to detect resistant parasites, which exploit the parasite's unique properties. We adopted
and refined this method early on to enable its use in tropical regions, and through this
approach, we became the first to identify Artemisinin-resistant parasites in Africa.
Moreover, by using next-generation sequencing, we sequenced the entire genome of these
parasites and compared them with malaria genomes from other regions. We found that the
resistance did not originate from Southeast Asia, as previously thought, but emerged
independently in Africa (Publication and press release in 2018). This discovery of Artemisinin-resistant
parasites in Africa has garnered global attention.
2) Moving forward – Expanding on Our Field Discoveries![]() Building on this discovery, our
research is now progressing to the next stage. The most important step is to clarify the
clinical effectiveness of Artemisinin treatment in patients with resistant parasites in the
areas where we discovered them. It’s a complex issue, but the Artemisinin-resistant
parasites we identified were found using an in vitro resistance test, where we cultured
parasites from infected patients alongside Artemisinin in a laboratory to assess their
resistance. However, it’s not just the drug that kills the parasites inside a patient’s body. The
patient’s own resistance and immune response also play a role. The strength and nature of
this “force” vary depending on the patient and the endemic area. Therefore, we are
conducting a study to treat patients with Artemisinin and determine the clinical effect of this
treatment. This study will reveal whether clinically resistant parasites have emerged in the
regions where we first identified them.
Building on this discovery, our
research is now progressing to the next stage. The most important step is to clarify the
clinical effectiveness of Artemisinin treatment in patients with resistant parasites in the
areas where we discovered them. It’s a complex issue, but the Artemisinin-resistant
parasites we identified were found using an in vitro resistance test, where we cultured
parasites from infected patients alongside Artemisinin in a laboratory to assess their
resistance. However, it’s not just the drug that kills the parasites inside a patient’s body. The
patient’s own resistance and immune response also play a role. The strength and nature of
this “force” vary depending on the patient and the endemic area. Therefore, we are
conducting a study to treat patients with Artemisinin and determine the clinical effect of this
treatment. This study will reveal whether clinically resistant parasites have emerged in the
regions where we first identified them.![]() We are also working to improve the in vitro testing method to detect Artemisinin-resistant
parasites. The current method requires skilled technicians to distinguish malaria parasites
under a microscope, which can lead to inconsistent results. We are improving this method
to make it simple and reliable for anyone to use, as well as developing a way to evaluate
resistance in a continuous (quantitative) manner. Since 90% of malaria cases occur in
Africa, it is crucial to detect resistant parasites early to prevent a major issue. Currently, no
malaria drug with the same effectiveness as Artemisinin is available, so it’s essential to
identify resistant parasites as early as possible and take preventive action. This is why
developing a “simple, stable, and universally applicable test method” is vital.
We are also working to improve the in vitro testing method to detect Artemisinin-resistant
parasites. The current method requires skilled technicians to distinguish malaria parasites
under a microscope, which can lead to inconsistent results. We are improving this method
to make it simple and reliable for anyone to use, as well as developing a way to evaluate
resistance in a continuous (quantitative) manner. Since 90% of malaria cases occur in
Africa, it is crucial to detect resistant parasites early to prevent a major issue. Currently, no
malaria drug with the same effectiveness as Artemisinin is available, so it’s essential to
identify resistant parasites as early as possible and take preventive action. This is why
developing a “simple, stable, and universally applicable test method” is vital.
____
・Laboratory Research![]() In order to validate the findings from our field research, laboratory
research is indispensable. Simultaneously, we are developing laboratory systems to predict
what will happen in the field. Below, I will explain the research activities we are engaged in
at the Department of Tropical Medicine and Parasitology, Juntendo University School of
Medicine.
In order to validate the findings from our field research, laboratory
research is indispensable. Simultaneously, we are developing laboratory systems to predict
what will happen in the field. Below, I will explain the research activities we are engaged in
at the Department of Tropical Medicine and Parasitology, Juntendo University School of
Medicine.
1) Validating Field Findings and Developing New Techniques for Early Detection of
Resistant Parasites![]() As mentioned earlier, our regular field surveys have led to new
discoveries. If these can be reproduced in the laboratory, they become more reliable
findings. Moreover, we aim to develop new technologies based on these discoveries.
With approval from the Ugandan government, we have been collecting malaria parasites
from patients in the field, freezing and transporting them to Japan. In our lab, we revive
these parasites and study how they became resistant to Artemisinin. By understanding the
mechanisms of resistance, we aim to develop drugs that target resistant parasites and
technologies that delay the emergence and spread of drug resistance.
We are also using population genetic methods to identify candidate genes related to
Artemisinin resistance in Africa. Once we identify mutations in the malaria genome that are
linked to resistance, we can introduce these mutations into susceptible parasites and test
whether they become resistant. This allows us to confirm whether specific mutations are
related to resistance. If they are, these genetic markers can be used for epidemiological
studies of drug resistance. These markers can be detected from just a drop of blood,
allowing for large-scale testing. By developing such new technologies, we can quickly and
affordably detect resistant parasites. When combined with the new in vitro methods
mentioned above, this will improve the accuracy of resistance detection.
As mentioned earlier, our regular field surveys have led to new
discoveries. If these can be reproduced in the laboratory, they become more reliable
findings. Moreover, we aim to develop new technologies based on these discoveries.
With approval from the Ugandan government, we have been collecting malaria parasites
from patients in the field, freezing and transporting them to Japan. In our lab, we revive
these parasites and study how they became resistant to Artemisinin. By understanding the
mechanisms of resistance, we aim to develop drugs that target resistant parasites and
technologies that delay the emergence and spread of drug resistance.
We are also using population genetic methods to identify candidate genes related to
Artemisinin resistance in Africa. Once we identify mutations in the malaria genome that are
linked to resistance, we can introduce these mutations into susceptible parasites and test
whether they become resistant. This allows us to confirm whether specific mutations are
related to resistance. If they are, these genetic markers can be used for epidemiological
studies of drug resistance. These markers can be detected from just a drop of blood,
allowing for large-scale testing. By developing such new technologies, we can quickly and
affordably detect resistant parasites. When combined with the new in vitro methods
mentioned above, this will improve the accuracy of resistance detection.
2) Predicting the Future – Developing a System to Predict Future Drug-resistant
Parasites in the Field![]() We are developing a laboratory system to predict future events in
the field. One method we use is laboratory evolution experiments, which have been
employed in several research labs with bacteria, viruses, and malaria to create drug-
resistant pathogens. By culturing malaria parasites with anti-malarial drugs, drug-resistant
strains will emerge. This method allows us to create resistant parasites that may appear in
the field in the future.
We are developing a laboratory system to predict future events in
the field. One method we use is laboratory evolution experiments, which have been
employed in several research labs with bacteria, viruses, and malaria to create drug-
resistant pathogens. By culturing malaria parasites with anti-malarial drugs, drug-resistant
strains will emerge. This method allows us to create resistant parasites that may appear in
the field in the future.![]() However, this method has a significant drawback: it can take several years to develop drug-
resistant malaria parasites. For instance, it took five years to generate Artemisinin-resistant
parasites using this approach.
However, this method has a significant drawback: it can take several years to develop drug-
resistant malaria parasites. For instance, it took five years to generate Artemisinin-resistant
parasites using this approach.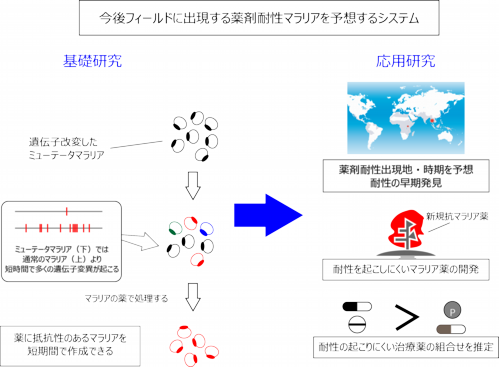
![]() To overcome this, we have introduced minor genetic modifications to malaria parasites to
make them evolve much faster than normal ones. These modified parasites, called mutator
malaria parasites, can develop resistance in a matter of weeks to months when exposed to
anti-malarial drugs. This innovative technique has already allowed us to isolate drug-
resistant parasites. We are using these isolated parasites to explore the mechanisms of
resistance and identify the responsible genes. This will enable us to prepare effective
diagnostic tools and treatments before resistant parasites emerge in the field.
To overcome this, we have introduced minor genetic modifications to malaria parasites to
make them evolve much faster than normal ones. These modified parasites, called mutator
malaria parasites, can develop resistance in a matter of weeks to months when exposed to
anti-malarial drugs. This innovative technique has already allowed us to isolate drug-
resistant parasites. We are using these isolated parasites to explore the mechanisms of
resistance and identify the responsible genes. This will enable us to prepare effective
diagnostic tools and treatments before resistant parasites emerge in the field.
3. Conclusion
![]() As mentioned above, our lab takes an integrated approach from both the field and the
laboratory, conducting comprehensive research that can contribute to malaria control
efforts. We are always accepting PhD and master's students, and we open recruitment for
postdoctoral researchers and professional staff when positions become available. We
prioritize diversity within our lab and recruit individuals with achievements in other research
fields. If you are interested, please contact us at tmita[at]juntendo.ac.jp.
As mentioned above, our lab takes an integrated approach from both the field and the
laboratory, conducting comprehensive research that can contribute to malaria control
efforts. We are always accepting PhD and master's students, and we open recruitment for
postdoctoral researchers and professional staff when positions become available. We
prioritize diversity within our lab and recruit individuals with achievements in other research
fields. If you are interested, please contact us at tmita[at]juntendo.ac.jp.